Read the Full Report
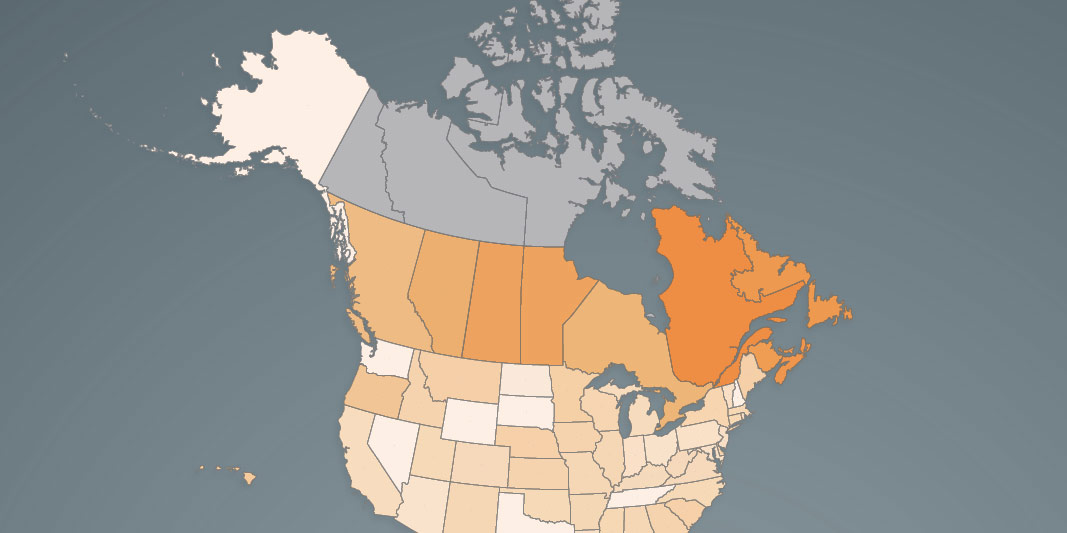
Read the Full Report View the Infographic - Income Tax Rate at CA$50,000
View the Infographic - Income Tax Rate at CA$50,000 View the Infographic - Income Tax Rate at CA$50,000 (Atlantic Canada)
View the Infographic - Income Tax Rate at CA$50,000 (Atlantic Canada) View the Infographic - Income Tax Rate at CA$75,000
View the Infographic - Income Tax Rate at CA$75,000 View the Infographic - Income Tax Rate at CA$75,000 (Atlantic Canada)
View the Infographic - Income Tax Rate at CA$75,000 (Atlantic Canada) View the Infographic - Income Tax Rate at CA$150,000
View the Infographic - Income Tax Rate at CA$150,000 View the Infographic - Income Tax Rate at CA$300,000
View the Infographic - Income Tax Rate at CA$300,000 Read the News Release - Canada
Read the News Release - Canada Read the News Release - Atlantic Canada
Read the News Release - Atlantic Canada